Dr. Dana Shani
Hype viscosity & elevated serum antibodies titers – surgical safety
Research Inquiry
70 y/o male was found to have prolonged PTT prior to surgery…work up revealed elevated titers of lupus anticoagulants and anticardiolipin antibodies and elevated IgM 3225 (norm 35-242) with elevated serum viscosity of 2.6 (norm 1.4-2.1). CT scan of CAP, NO lymphadenopathy. Pt needs to undergo elective abdominal surgery. Is he safe to have surgery with the elevated IgM, elevated serum viscosity, and high titers of lupus anticoagulants?
Conclusion
The literature and guidelines that we reviewed in our research are suggesting that the presence of antiphospholipid antibodies like Lupus anticoagulant & anti-Cardiolipin can occur in healthy individuals, and the first essential step in the management is understanding the risk of thrombosis and eliminating reversible risk factors known to increase risk of clotting.
In the case of surgery, aPL-positive is not a complete contra indication for surgery, but it is associated with a risk of thrombosis and may also elivate the risk of bleeding, especially in High risk patients with the presence of LA. As a result, if the surgery is not urgent, we advice conducting complete and comprehensive lab tests to rule out transient etiologies and to ferture pursue a diagnosis (with a 12 weeks confirmation period). If the surgery is urgent and\or there are persistent aPL lab results, a risk stratification and prevention strategies should consider traditional cardiovascular and venous thrombosis risk factors, other comorbidities, systemic autoimmune diseases, and the aPL profile during preoperative assessment of thrombotic risk. In addition, the least invasive option should be pursued in order to minimize the risk.
There is a lack of evidence in the literature about the surgical management of patients with high blood viscosity, but the main general risk that can be relevant to the case is mucocutaneous bleeding – a symptom that was not mentioned in the clinical background of our patient.
Medical Meta Findings
- Elevated serum Lupus anticoagulant & anti-Cardiolipin:
-
According to an article[1] published in “Antiphospholipid (aPL) Syndrome” book in 2012, Antiphospholipid antibodies can occur in otherwise healthy individuals or in patients with other autoimmune disorders such as systemic lupus erythematosus (SLE). Having a positive aPL test does not mean the person has APS; 30–40% of SLE patients may have aPL, but only a small percentage develop APS. For all aPL-positive patients with or without SLE, whether or not they have had a blood clot in the past, the first essential step in the management is understanding the risk of thrombosis and eliminating reversible risk factors known to increase the risk of clotting.
In most cases of Asymptomatic Antiphospholipid Antibody Positivity, the antibodies are usually incidentally discovered on testing done for other reasons by their doctors, as aPL may cause abnormal activated partial thromboplastin time (aPTT), which is a clotting test used to determine the bleeding risk before surgical procedures – some patients may be found to have aPL during the preparation period for surgical procedures. Individuals with persistently positive aPL require close attention during surgical procedures, and may often receive low doses of blood-thinning medications to prevent clots, and they should always consult with their doctors before elective surgeries. This is of greatest concern in those patients who are usually on anticoagulation and must stop this treatment before the surgery to avoid bleeding risks. These patients should be watched carefully for signs of clots that can be induced by surgical procedures, immobilization, and/or intravenous line placements. Anticoagulation with heparin should begin as soon as possible after the surgery.
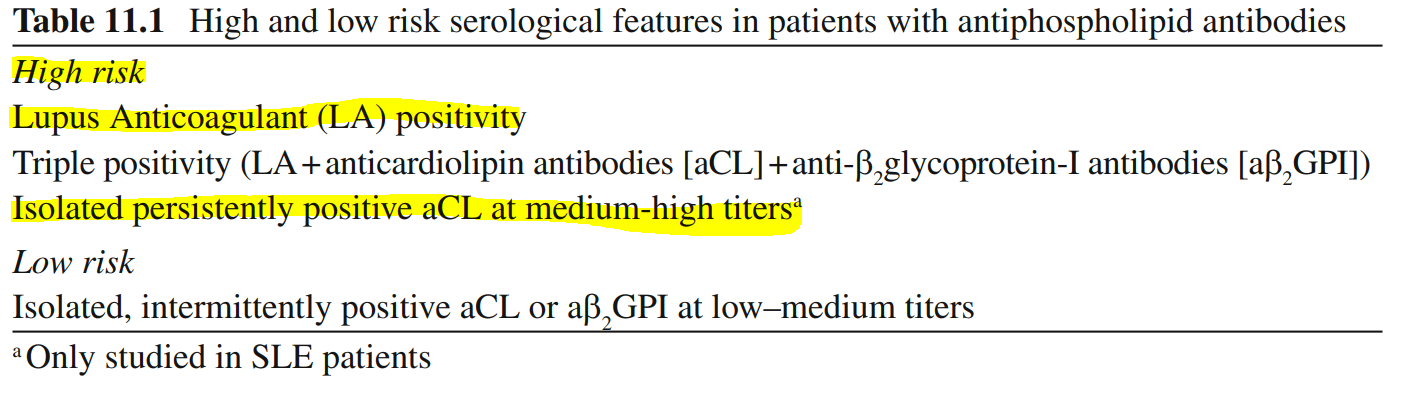
Those recommendations are also backed up by the Task Force Report [2] on the Management of Thrombosis in Antiphospholipid Syndrome, published in the same book, noting that all aPL carriers receive thromboprophylaxis with usual doses of LMWH in high-risk situations, such as surgery, prolonged immobilization, and puerperium, especially in the case of our patient, which is considered a high-risk patient:
-
According to the Guidance[3] from the Scientific and Standardization Committee for lupus anticoagulant/antiphospholipid antibodies of the International Society on Thrombosis and Haemostasis, published in The Journal of Thrombosis and Haemostasis in 2020, Lupus anticoagulant (LA) is one of the three laboratory criteria for the identification of the antiphospholipid syndrome (APS), that can alter a prolonged PTT test. For that reason, a positive mixing test result (as described in the article) should be confirmed after 12 weeks to exclude transient Lupus anticoagulant presence, induced by infection or drugs.
It is important to note that Lupus anticoagulant has the best-established connection to APS-related clinical manifestations, like hypercoagulability, which is a major risk factor in surgeries. As a result, we advise further investigating the patient’s thrombotic events history and other clinical and laboratory manifestations that can help confirm or eliminate APS.
-
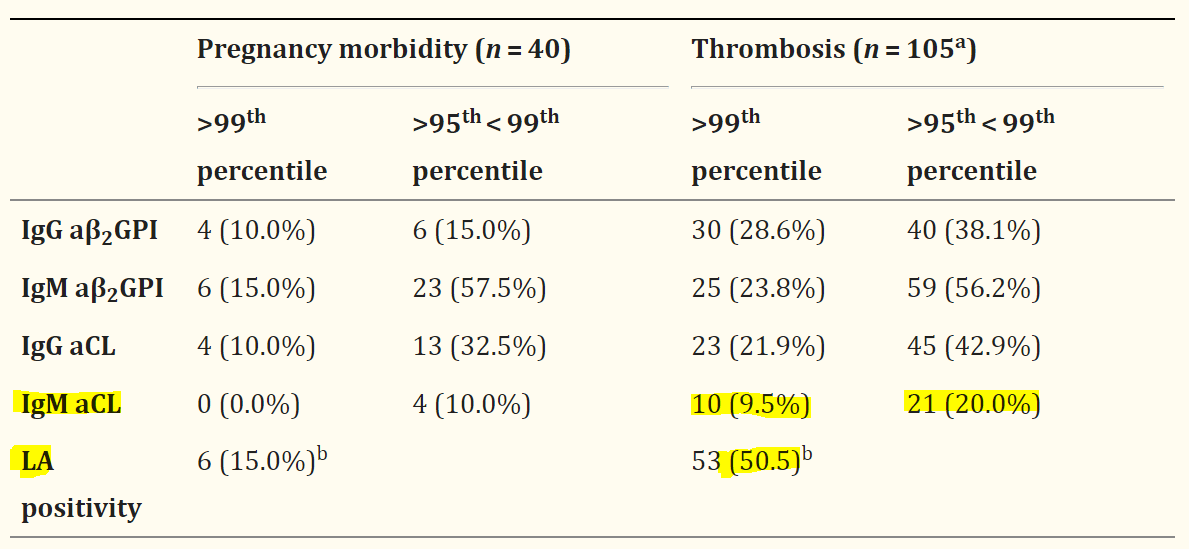
According to the laboratory criteria[4] for antiphospholipid syndrome published in The Journal of Thrombosis and Haemostasis in 2018, Anticardiolipin and beta2-glycoprotein I antibodies are also linked to thrombosis, and according to the paper there is a stronger association of IgG with thrombosis compared to IgM, but there is still a significant association for IgM too. It is advice in the criteria to also messure the levels of beta2-glycoprotein I antibodies, because triple positive patients are at high risk of thrombosis. 12 moth reconfermetion is advised also In triple positive patients.
-
An article[5] published in Lupus journal in 2013 reviews the ways of diagnosing antiphospholipid syndrome in routine clinical practice. It is mentioned in the article that there are many clinical manifestations associated with persistent antiphospholipid antibodies like Lupus anticoagulant and anti-Cardiolpin, including infections, drug use, immune thrombocytopenia, livedo reticularis, migraine, valvular heart disease, and cognitive dysfunction. The researchers also showed the distribution of antiphospholipid positivity by clinical diagnoses in a cohort of 126 patients. The percentage of positive tests and median antibody levels (>99th or > 95th < 99th percentile) were given for each clinical group. As shown in the table, there is a link between high titers of Lupus anticoagulant and Anticardiolipin to Thrombosis.
-
A way of perioperative management of Antiphospholipid Antibody-Positive patients is described in an article [6] published in Current Rheumatology Reports in 2014. According to the researchers, a “second-hit hypothesis” proposes that aPL positive patients require an initiating event, for example a surgical procedure, to develop thrombosis. Because thrombosis is multifactorial, risk stratification and prevention strategies should consider traditional cardiovascular and venous thrombosis risk factors, other comorbidities, systemic autoimmune diseases, and the aPL profile during preoperative assessment of thrombotic risk. Furthermore, given the high risk, elective surgery should be strongly discouraged and the least invasive option should be pursued, and when surgery is elective, the patient should participate in the creation of a thrombosis prophylaxis plan and he should be familiar with all aspects of medical and physical thrombosis prevention, including early mobilization after surgery.
In addition to thrombotic events, aPL-positive patients at risk of bleeding from excessive anticoagulation, and are sometimes susceptible to bleeding secondary to their underlying condition. For example, Approximately 20% of patients with APS develop thrombocytopenia. Prolonged aPTT and minimally prolonged PT attributed to aPL are not contraindications for surgery; marked PT prolongation (internal normalized ratio [INR]>2.0) should prompt further evaluation before the procedure if possible.
According to the writers, there are four steps to reduce the perioperative thrombosis risk:
1. Minimize periods without anticoagulation.
2. Restart postoperative anticoagulation as early as possible.
3. Use physical methods in addition to pharmacologic methods.
4. Encourage postoperative ambulation and mobilization as early and as much as tolerated.
-
The following patient-oriented article[7] was published on the website of the Hospital for Special Surgery in 2012 and can be presented to our patient as a reliable and comprehensive data source.
-
According to an article[8] published on Frontiers in Oncology in 2020, the predominant symptoms of Hyper viscosity syndrome are mucocutaneous bleeding, ophthalmologic, and neurologic. Hemorrhage typically occurs in small venules associated with increased viscosity in areas with minimal supporting tissue, such as the nose and oral cavity (Epistaxis, gingival bleeding, Gastrointestinal bleeding).
-
Another article[9] published in Blood journal in 2018 mentions that asymptomatic patients with an elevation in the serum viscosity do not require plasma exchange, and the majority will have other indications for therapeutic intervention.